Cancer – A common enemy, implacable and increasingly present in the world’s population
When Dentistry is evolved, predictable and safe, it has the obligation and moral duty to leave the trenches of conformism and move onto the battlefield, where the challenge is daily and permanent. It is up to us, as qualified professionals working in an area as specific as Oral Rehabilitation, to find solutions that are not always possible at a first glance, at a first consultation, at the first examinations, what the Anglo-Saxons call the art of:
“to think out of the box…”
Which, in a quick and direct translation, leads us to:
“to think outside the box…”.
Thinking outside the box is nothing more than coming up with unorthodox solutions, or at least ones that are not so obvious or probable, but which, especially in the context of medicine, have to be tested, safe and ethically correct solutions.
We haven’t invented anything, we haven’t created anything, we haven’t pioneered anything. There are no secrets. Just the will to be competent and make a difference.
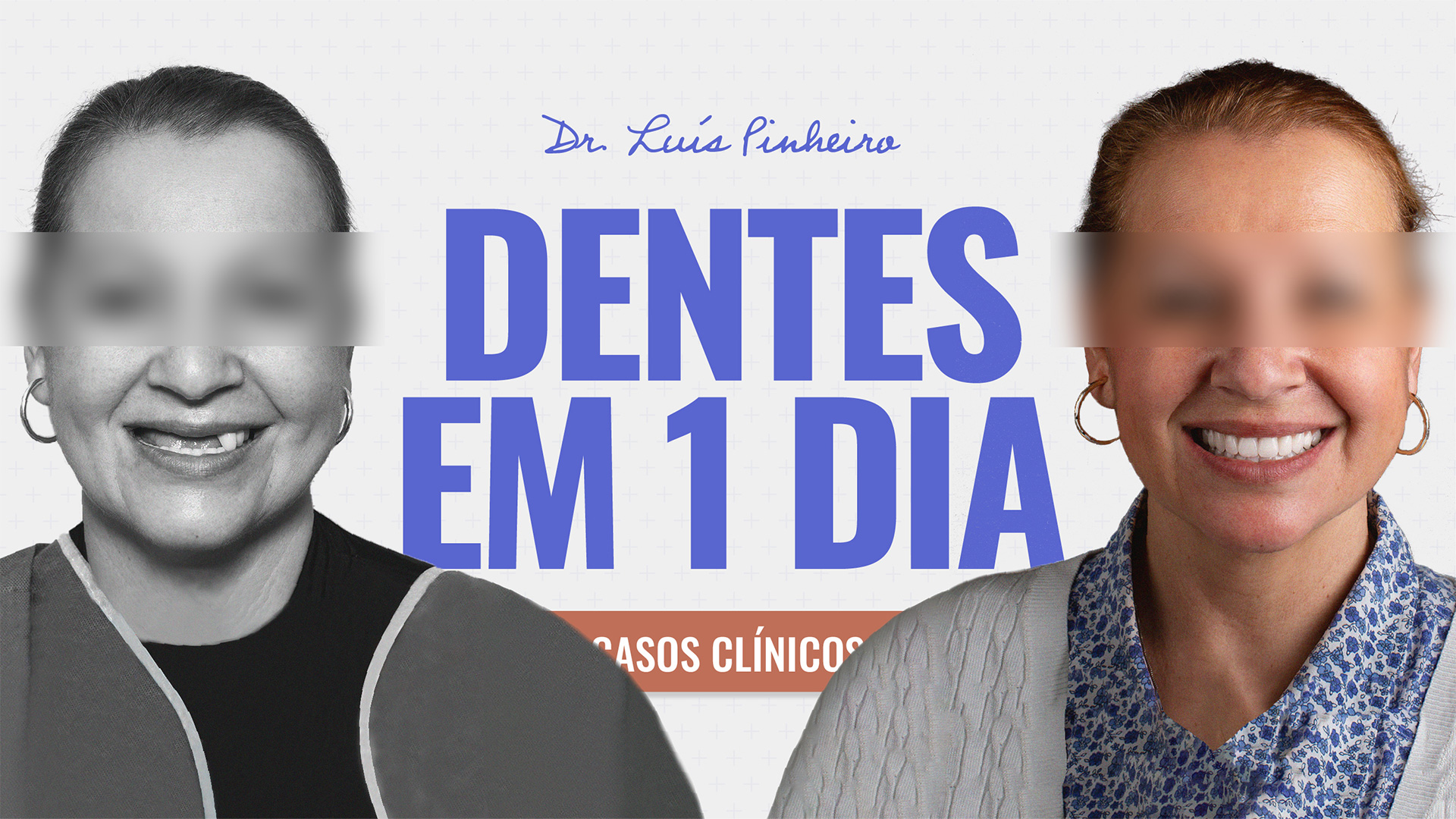
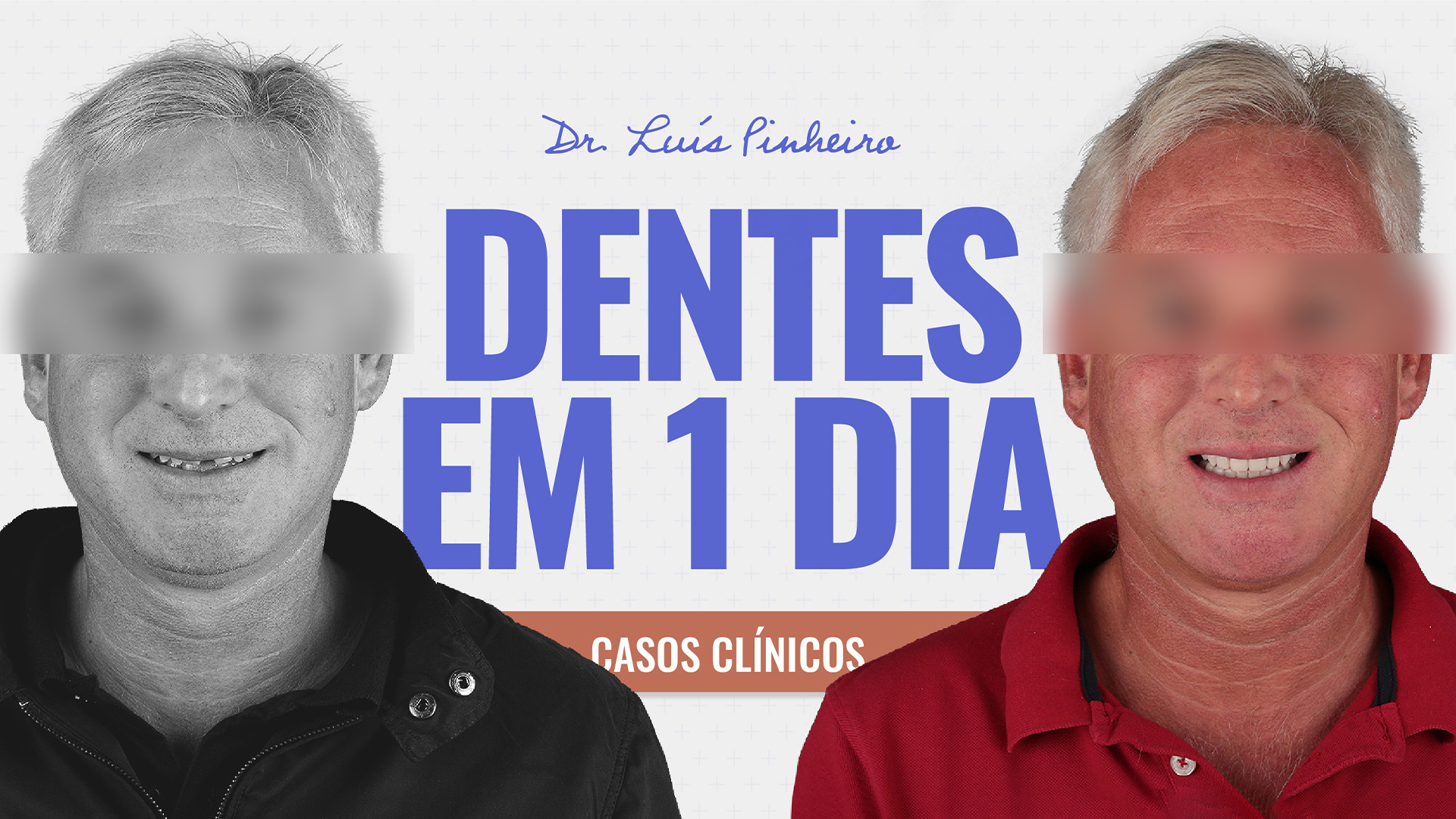
What we are very proud of in this Team is our exclusive dedication to this project. What exists in this Team is a group of health professionals and others who focus on each patient and make this treatment plan an authentic, unique and careful endeavour, which we are proud to show.
As a team, it’s up to us to bring together all the knowledge and experience we’ve accumulated over the years, to be at the “cutting edge” of the best of what’s being done around the world today, to have state-of-the-art facilities and equipment, and with all these skills together, to be able to aim for a final product that pleases the patient first and foremost, and of course, our entire team.
Cancer Epidemiology
In the case of cancer, recent studies show that 1 in 4 people will develop cancer in their lifetime, and of those, 1 in 3 will die from the disease. As cold and violent as these figures may be, everything becomes even sadder and more violent if we remember that each number corresponds to a person, a patient who is someone’s father, someone’s son, someone’s husband and friend.
People, who are generally wise, often say: “it’s one of those things that when you don’t die of the disease, you die of the cure…”
This applies in part here, since cancer treatments are usually violent, deforming, especially in the Maxillofacial area and in overall terms of the body, both Radiotherapy and Chemotherapy leave sequelae and conditioning factors that can last from 6 months to several years after the treatment cycles.
Patients are living longer and have a greater number of illnesses.
More and more of our patients are multi-medicated, with multiple pathologies, some chronic, others with an acute clinical condition, some controlled, others not so much, and it’s not enough for us to look the other way and pretend that we’re not facing a complicated situation, in order to often, as we see out there, proceed with invasive treatments in patients for whom said treatment would not be the first choice, the safest, the most ethical, the most necessary.
What I mean by this is no more than that for each patient there is a specific, rigorous treatment plan, with clinical and surgical concerns, and that we cannot irresponsibly, facilitatingly and ignorantly advocate the same treatment for all patients.
Current guidelines
Among colleagues we often exchange ideas, clinical cases, opinions, concerns and opinions, and something we often comment on is the fact that the more we study, the more we know, the more careful and concerned we are about possible, common and rare complications, and we are not in a position to risk our professional credentials in the slightest, much less, and more importantly, each patient’s most precious asset, their health and quality of life.
The contemporary trend in medicine is to classify health as something more complex than the simple absence of pain or illness, but rather as a state in which there is physical and psychological well-being and where the patient’s quality of life improves with a given treatment. (free adaptation of the definition from the World Health Organisation – WHO)
The subject of my thesis and research project at the University of London was, in general terms, the development of instruments to assess our patients’ Quality of Life before and after surgery and after the end of treatment.
With this, we collected valuable data on the impact of the treatments on our patients’ daily activities, and on the way they relate to their families, friends and work colleagues, if applicable.
What the future holds
We live in an incessant search for scientific knowledge, for improved techniques, so that we can give each patient the best possible treatment at a specific moment in their life and with the constraints that face our Clinical Team, in order to increase our patients’ Quality of Life.
There are cases, however, in which treatment is not possible at that moment and the best therapeutic decision is not to treat, but to postpone, waiting for more favourable pathophysiological and psychological conditions.
Communication between colleagues, between different specialities, between different Treatment Centres is essential for the clinical safety of patients, exchanging medical opinions, consulting the entire clinical file, sending tests, requesting additional analyses and tests that may be useful and necessary to define clinical conditions and make appropriate treatment plans.
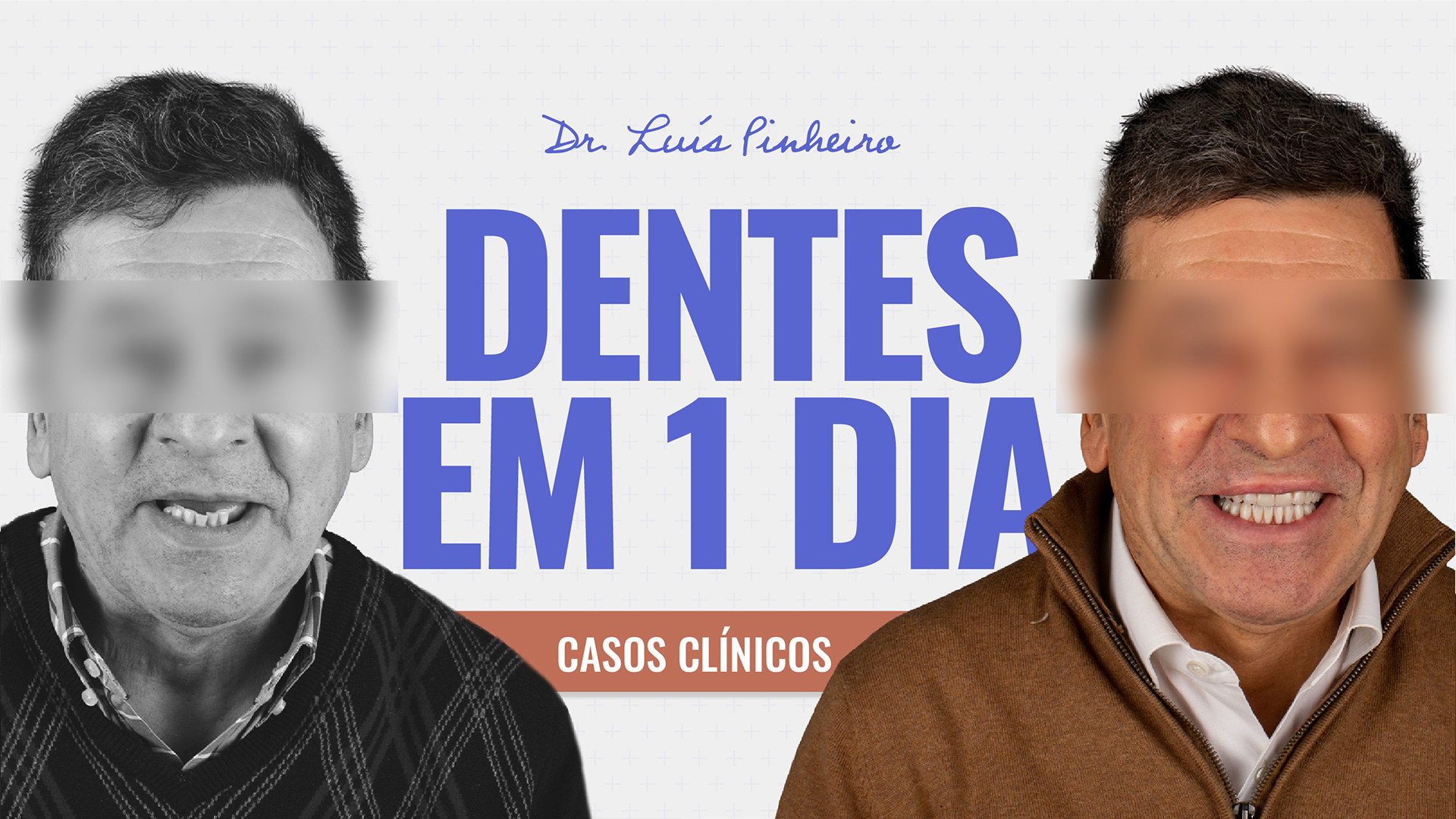
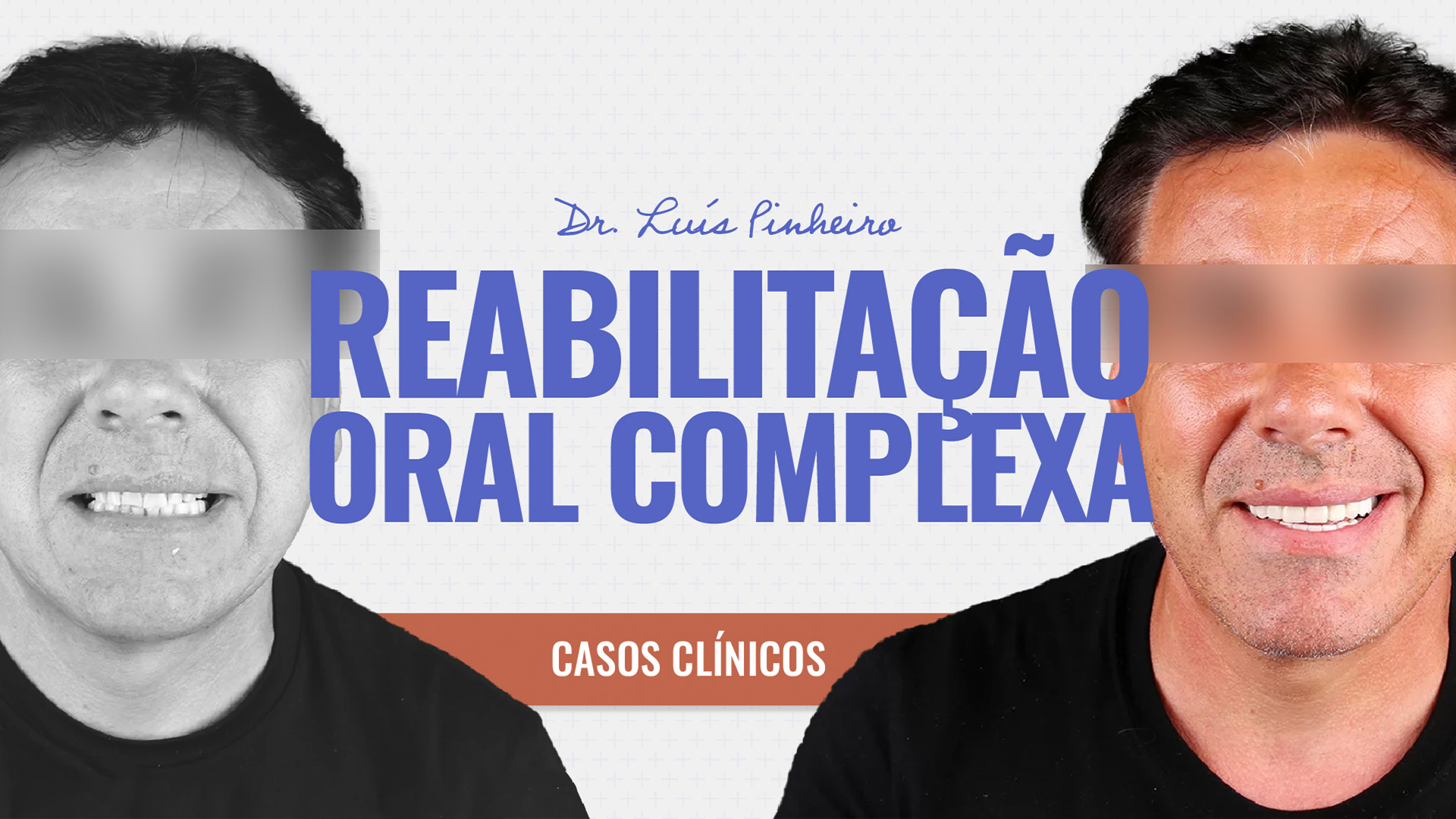
We recently published a case of one of our patients who has been fighting this great enemy that frightens us so much: cancer. After consulting the patient’s clinical file and talking to the oncology team that follows the patient, which, to be fair, was phenomenally willing to provide us with all the clinical information requested by our clinic and which, together with us, in a shared decision and responsibility, helped us to help the patient and find the best possible solution, at this specific moment, within the parameters of medical rigour, clinical safety and excellence.
Being aware and responsible in the medical profession.
We must always be cautious about criticising the work of other colleagues, since we are in a medical field in which our colleagues often work in unfavourable conditions and with clinical constraints, with which we work towards a compromise solution to carry out the best possible treatment to increase, to restore the Quality of Life of our patients.
I’ll end by thanking you for your attention and willingness to read this text, but even more importantly, I’ll end by thanking you for the example of courage, determination and love of life that cancer patients give us, showing humanity that we often give importance to situations that aren’t even a waste of our time.
See you soon and don’t forget to be happy. After all, smiling doesn’t hurt…
If this is the case, if smiling causes you pain, nausea or imbalance, consult your dentist.
Until next time!