When we start a text, a communication or a lecture with a key phrase like the one above, it has a purpose:
To draw the attention of the readers, or the listeners.
In this situation, the attention is drawn not to the bone grafts themselves, because they do exist, but to those who advertise and sell them, where everything is a graft, where any bone manoeuvre or filling of a defect, even a non-existent one, is pompously called a bone graft.
Whether it’s for commercial or business purposes, or for disproportionate ego boosts, we unfortunately see a lot of bone grafts advertised, sold or promised to patients these days, but grafts performed with rigour, purpose and surgical skill, I say, very honestly and in the name of my professional class, in the name of medical codes of ethics and in the name of surgical Legis Artis, I say and repeat, that I have seen very few colleagues throughout my career.
I’m not saying that only I or my team know how to do it, because if I did, it wouldn’t be surgery, surgery as a science, but surgery as a skill, as empiricism, and that’s not medical, it’s a skill, with all the medical and scientific rigour that it doesn’t have.
A medical or surgical manoeuvre has a learning curve, which depends on the experience and knowledge acquired by the surgeon throughout their clinical practice, but which each and every informed, trained and responsible surgeon is capable of performing once they have reached and mastered their learning curve. So if any of us surgeons or doctors tell you that we have a technique that only we can master and do, it’s not science, it’s juggling.
And with that, I come to the chapter of Oral Surgery that talks about Bone Grafts.
We need to place bone where it doesn’t exist and remove it from where it isn’t needed or where we have too much. So in surgery, we either have to place bone grafts or we need to regularise, change the shape of or reduce the amount of bone.
Handling bone, whether it’s cutting it, wearing it, drilling it, screwing it, physically manipulating it outside the body and moving it from one place to another, requires a high level of knowledge, training, expertise and technology, and the full involvement of a team trained to carry it out. I’m not talking about the anatomical, physiological, biological and genetic knowledge that is implicit in those who call themselves doctors.
So bone grafts are not a myth and they work very well.
Then there’s all the information and counter-information about the origin of grafts, with a whole variety of origins, from a miraculous “little powder” to some phenomenal membranes that you just have to add boiling water to and you’ve got soup…
Irony aside, and forgive my exaggeration, both in the training courses I attend as a trainer, at the University of London where I continue my surgical training, and over the last 10 years where I have dedicated myself exclusively to oral surgery and its clinical practice, there have been countless cases of grafts that were unsuccessful, either due to planning errors, errors in the material chosen, errors in the surgical technique adopted, infection, smoking, lack of hygiene on the part of the patient, or simply not being indicated due to the patient’s medical history.
Without wishing to go into depth from a medical or surgical point of view, since that is not the intention of this document, and because instead of clarifying, I run the risk of further complicating a subject that in itself is already complex and the source of countless communications, scientific articles, book chapters, medical journals, conferences, postgraduate courses, master’s degrees and doctorates.
So I shouldn’t complicate its description and advice, nor should it be easy to use or trivialise, as I’ve seen a graft simply be a matter of placing a bit of material in a defect, or applying a membrane over bone, whether artificial or autogenous (from the patient themselves) and that’s it, with no regard for the properties of the materials or their behaviour in the body.
Where does the graft come from?
Is it of animal origin?
Is it from a cadaver?
From the patient?
Which is best?
We’re starting to get to the point where, in addition to the surgical technique to be chosen, we have to talk about the type of graft, the type of material or its origin.
The graft can be of synthetic, animal or human origin.
From the point of view of function in dentistry, we now have at our disposal a range and variety of materials that also allow us to obtain different results and which often complement each other.
We have materials that facilitate or induce bone formation, which is why they are called osteoinductive.
We have materials that conduct bone formation from one place to another, hence the name Osteoconductors.
Synthetic filling materials form matrices, skeletons to allow the body to grow through them, allowing them to be invaded by blood vessels and nerve endings that will bring oxygen and nutrients to the site, as well as biochemical and cellular markers so that the whole process of bone formation, Osteoinduction, can begin, in order to obtain Osteogenesis (bone formation).
It is part of my daily area of clinical and surgical intervention, as well as an integral part of my curriculum of study at various universities in various countries, Lisbon, Porto, Barcelona, Paris, São Paulo, London, where I have been to date, and it is probably and will continue to be one of the areas of greatest study and involvement of the international scientific class.
I don’t want to and can’t go any further in a blog post in terms of specific and specialised medical and scientific knowledge, but I will leave more material here so that you, dear reader, have topics of interest that you can investigate on your own or in books or on the internet, which is normal practice these days.
The graft can be of animal origin such as bovine, porcine, equine and so on.
The use of cadaver banks has been used in the past and is still used today in some scientific centres, but according to the current literature, for the type of bone graft surgery in Oral Surgery, it is not in fact the most widely used.
We have the patient’s own bone at our disposal, the so-called autogenous graft.
Here we manage each patient’s bone heritage and take bone from where it exists to where it doesn’t exist.
As donor sites, we have various anatomical regions, from the iliac crest to the rib, tibia, perineum and skull cap, but in my clinical, medical and surgical opinion, I repeat, in my opinion, obviously based on years of experience, mine and those I’ve learnt from, and on studies, in articles, in Evidence-Based Medicine, I can conclude that this type of donor area is justified today for major reconstruction of the face and jaws, in Maxillofacial Surgery after trauma, and after oncological pathology using resective surgery.
The most commonly used donor areas for Oral Surgery and Implantology, which allow us to have greater treatment predictability, are found intraorally, using grafts from the ramus of the mandible, the chin and the maxillary tuberosity.
As with any medical procedure, it is essential that the surgical technique is carried out by a medical professional/surgeon who has been trained for this purpose and whose curriculum is suitable for this purpose. I know it sounds too obvious, but believe me, it’s not that obvious.
By way of conclusion, I’ll leave you with a little provocation:
Dear readers, you can try searching the internet and the literature, or even easier, there are professionals who have studied and studied for years, who have dedicated a lifetime to medical and surgical practice, who generally have a space where they receive you, in their clinics and with a specific time for any and all questions, the so-called consultation.
My recommendation here:
Ask your questions, make an appointment with us or your dentist.
However, there are situations in which, no matter how great the graft, the defect, the atrophy of the upper jaw, in this case, is so great that we have come to realise over the last 15 years, and even more so over the last 10 years, that the graft solution is not suitable for everyone or everything and we have another type of approach at our disposal:
Zygomatic Implants
But that’s another story…
It will be my next topic on this blog.
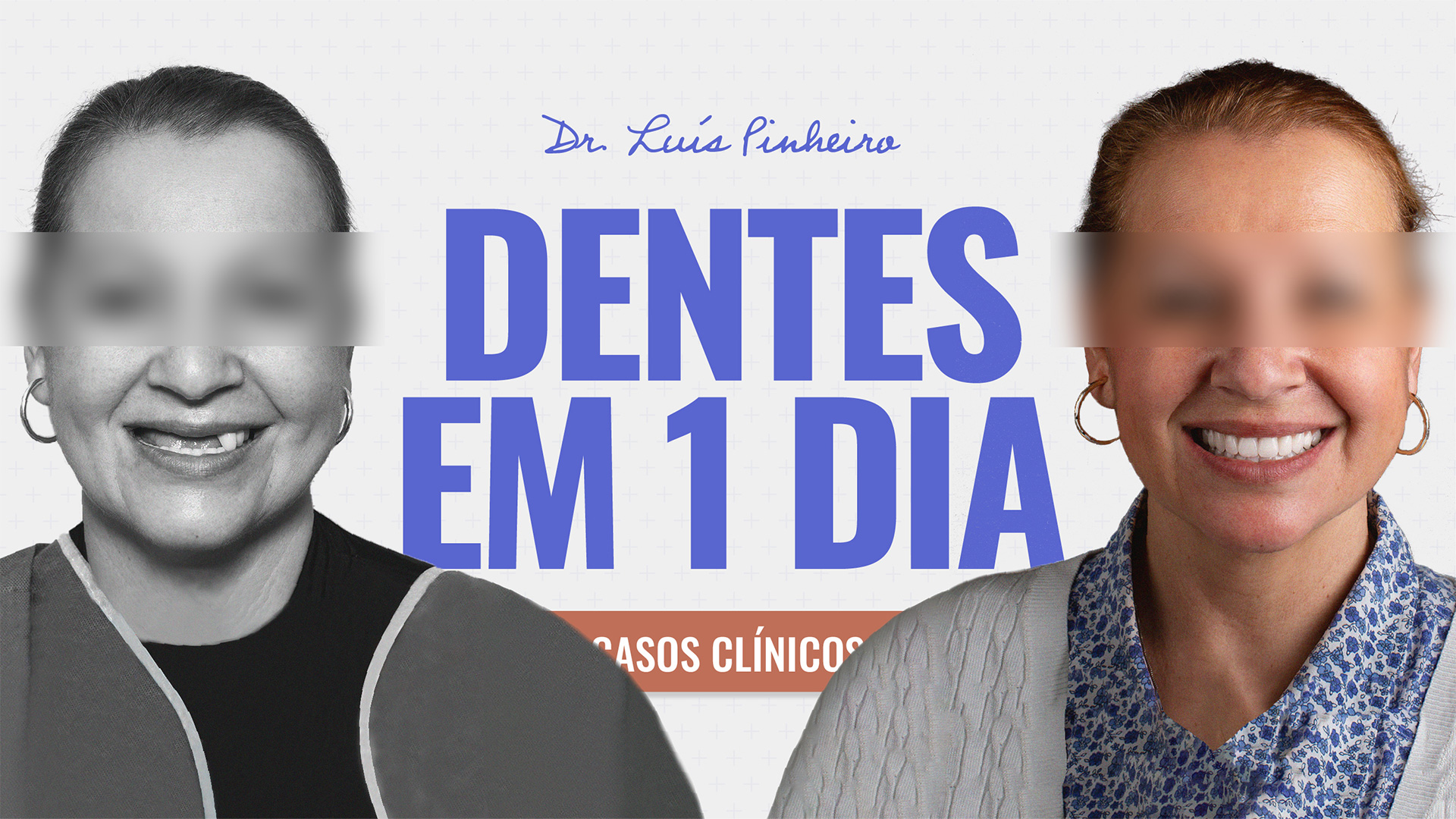
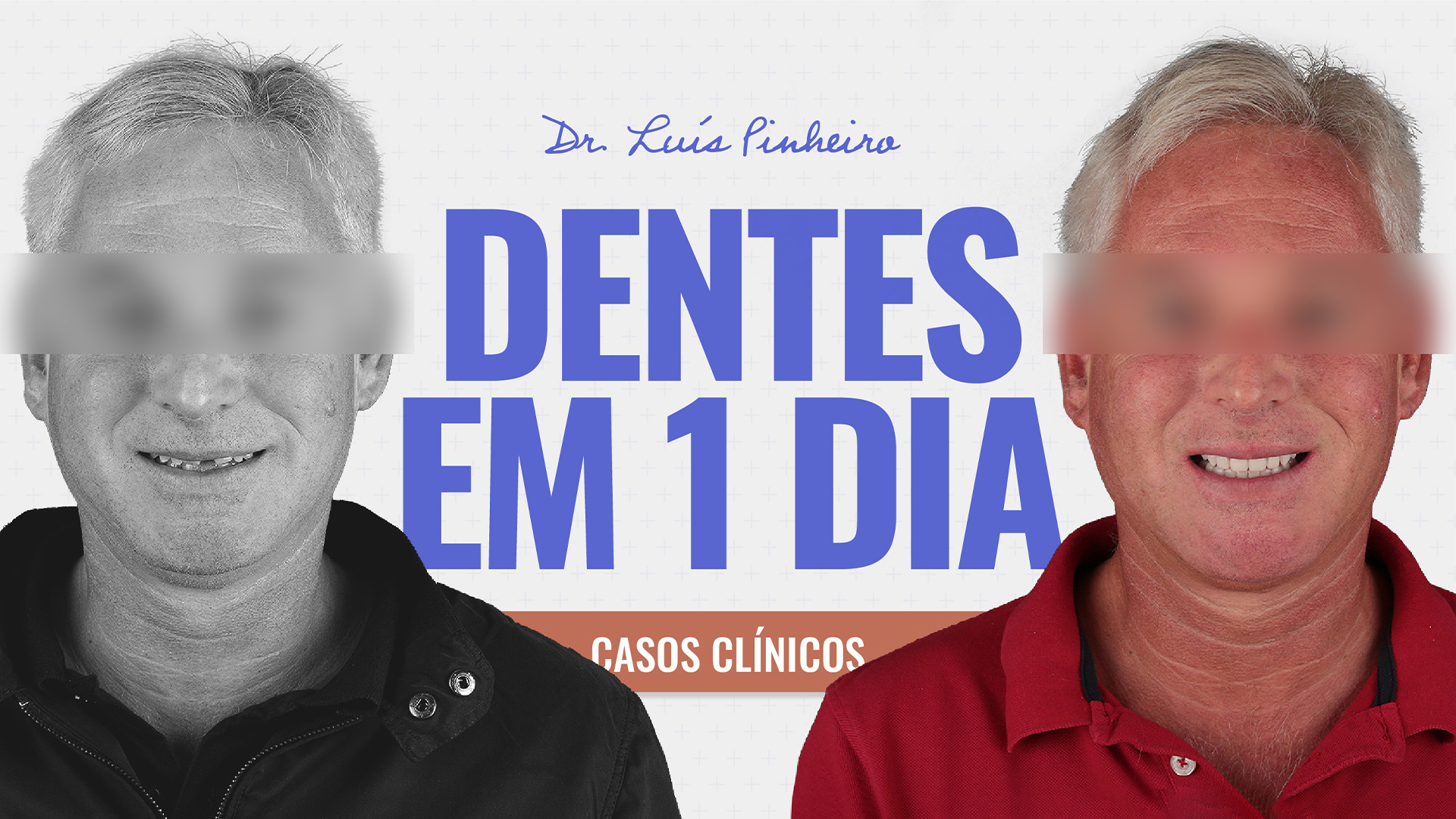
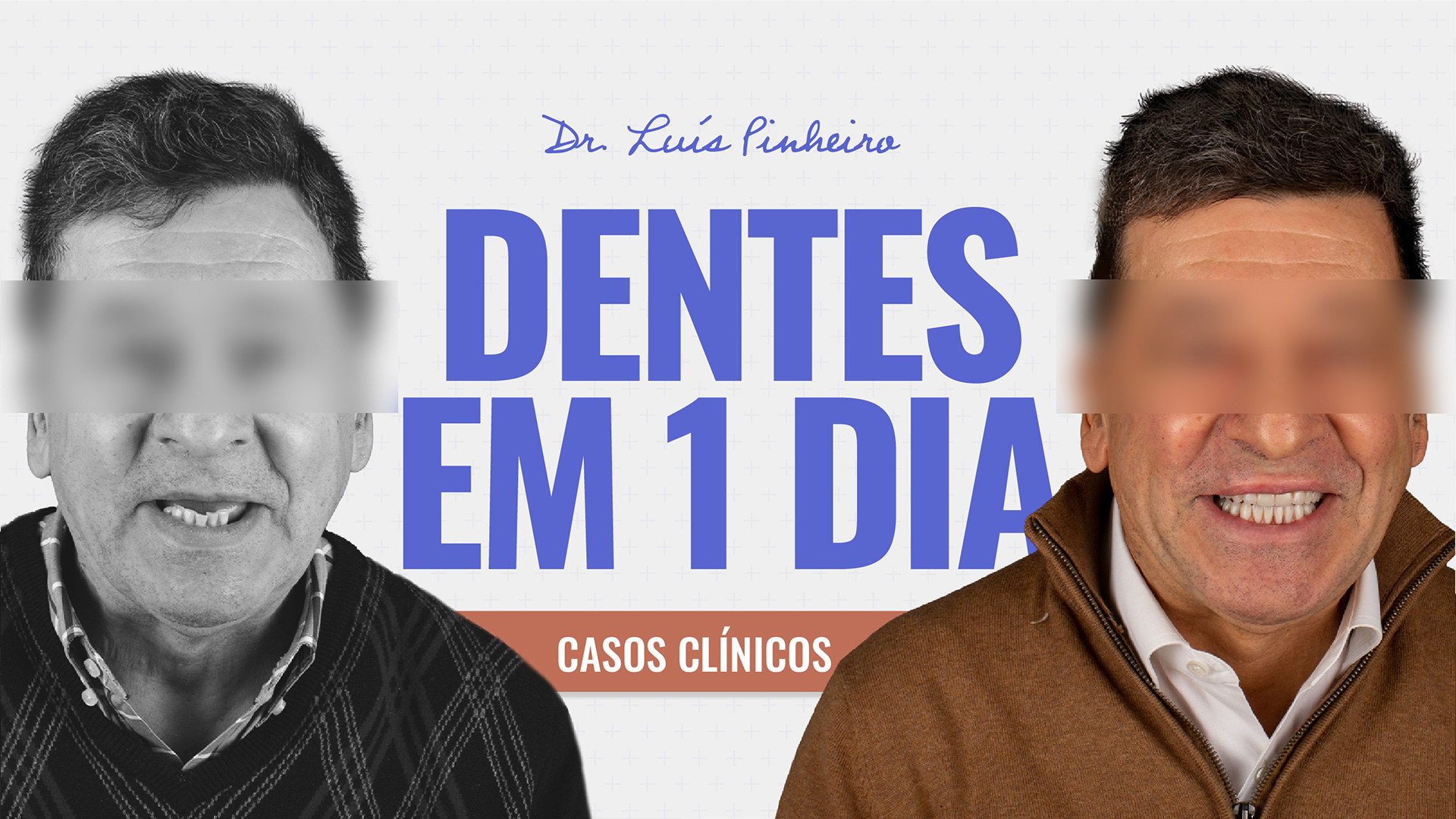
See you soon and don’t forget to be happy. After all, smiling doesn’t hurt.
If it does, if smiling causes you pain, nausea or imbalance, consult your dentist…
Until next time