WHAT ARE ZYGOMATIC IMPLANTS?
Let’s start by locating ourselves:
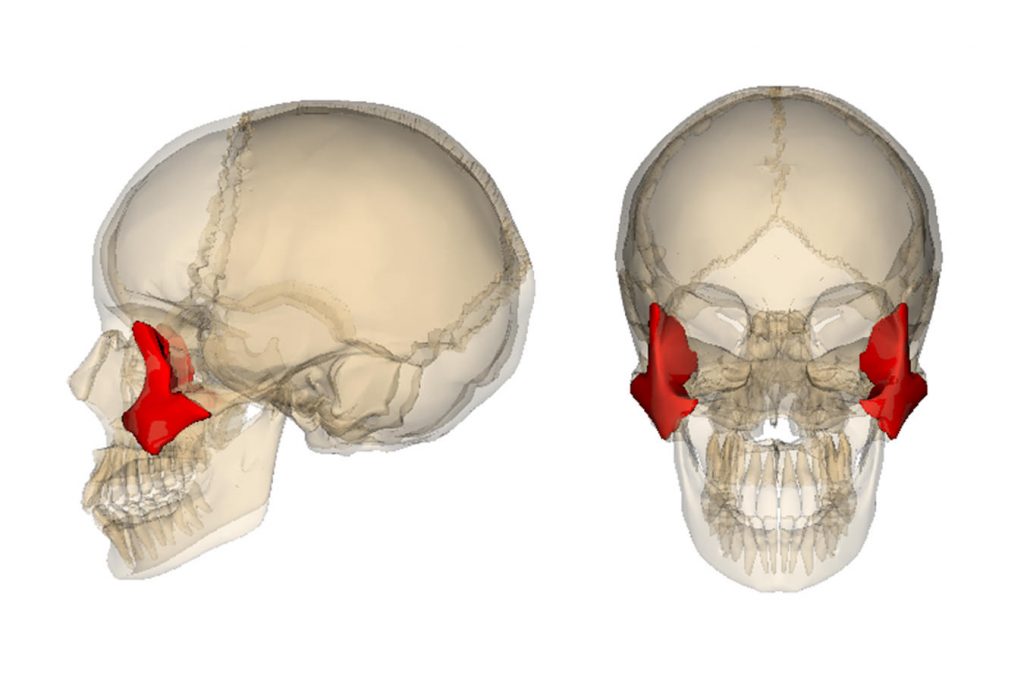
Zygomatic implants have this name because they are implants placed in the zygomatic bone. For those of you who are older, I’m sure you remember the old Anatomical Standard (before 1998), in which the Zygomatic bone was called the Malar bone. It’s not wrong to call it the Malar bone, from a lay and social point of view, but in medical and surgical terms the bone is now called the Zygomatic bone.
The surgical technique is called Zygomatic Implant Placement or Zygomatic Transfixation, as can be found in scientific literature.
In this context, I’m not going to go into the description of the various surgical approaches, nor the type of research that is being carried out today, both at a medical and surgical level, in order to make surgery ever safer, more predictable and with results that allow for ever better and more appropriate Oral Rehabilitation for our patients, as well as the scientific research in which I am involved in various projects, whether it’s training in Portugal, where I represent the implant brand we work with at CERO, or the study and research I’m currently carrying out at the University of London, as part of my Masters in Oral and Maxillofacial Surgery. I’ll be happy to go into more detail with you later, and why not even share results and advances in this area, but I don’t think the purpose of this text and this blog will take you down that road
Instead, I’m going to approach the subject in a less academic, surgical or scientific way, and more clinically, practically and in terms of Oral Rehabilitation.
A brief historical introduction
Transzygomatic fixations have been used for several decades. They were first used in surgical and prosthetic rehabilitation after tumour resection in patients who had lost a large part of the anatomical structures that make up the face, such as the jaws, orbits, nose, etc. Their use was part of a prosthetic complex that fixed the prosthetic obturators, together with another type of implant that were bone fixing screws so that medicine could give these patients back some quality of life after such mutilating surgeries and where patients need to recover their quality of life, in part or almost completely. Even in terms of scientific publications, there is a test, a scale to measure the Quality of Life of patients after surgery and rehabilitation.
In my research work, my team and I also use a modification of this questionnaire to better understand where we can and should invest and research to improve the less positive aspects and maintain or even further improve the already positive aspects of this type of Oral Rehabilitation.
This type of Oral Rehabilitation, in prosthetic terms, is very similar to the type of Fixed Total Rehabilitation that we do for the totally edentulous.
I’m opening a slight parenthesis here to try to explain to those reading this what we doctors classify as total edentulousness in terms of current dentistry, which is accepted and based on the principles of scientific evidence-based medicine:
– Patients who no longer have any teeth or dental roots/fragments in their jaws,
– Patients who have some teeth, but these no longer have any function due to their lack of support, incorrect size or position, or because they have chronic inflammatory and/or infectious symptoms.
When this situation manifests itself in both jaws, it is total edentulism.
When the situation manifests itself in only one jaw, it is upper or lower total edentulism, depending on the jaw in question.
In the case of Zygomatic Implants, we are talking about their applicability only to the Upper Jaw, due to the anatomical proximity of the Zygomatic Bone to the Upper Jaw (Maxilla).
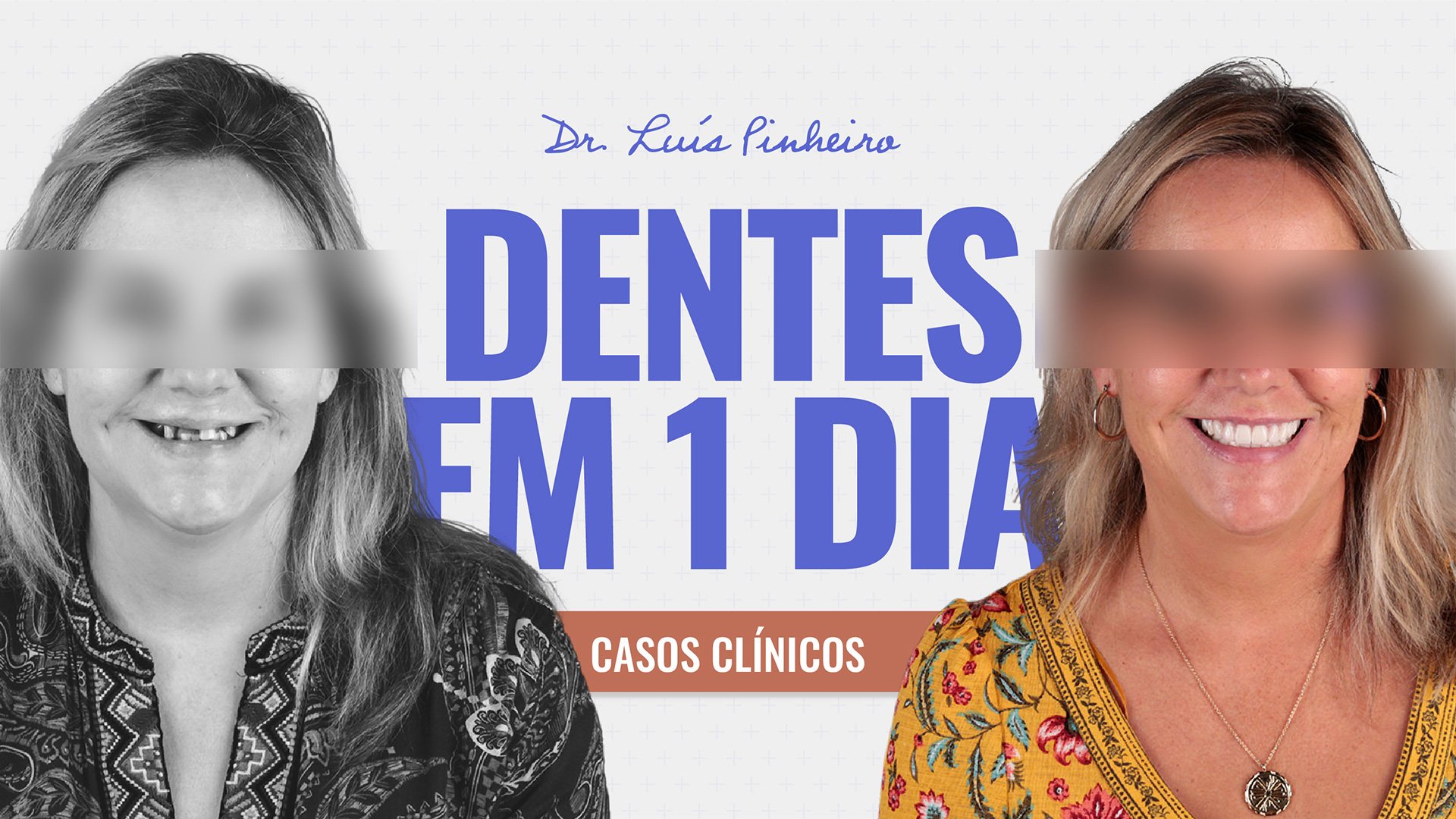
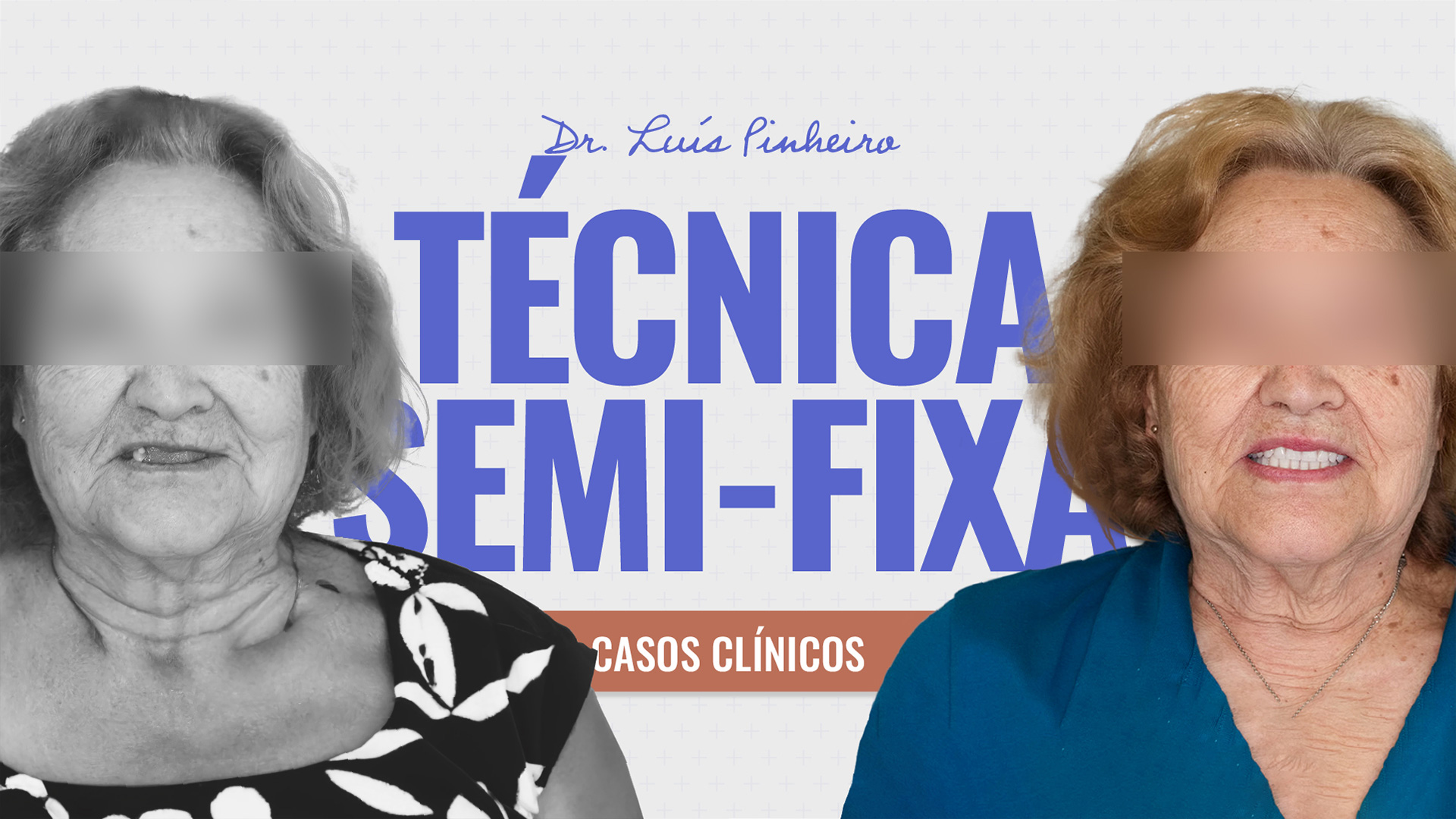
Over the last few years, surgical techniques and oral rehabilitation materials and techniques have evolved so that the final work, i.e. what the patient actually has in his mouth, can enjoy, eat, speak, re-establish muscle and soft tissue shapes and dimensions and, in aesthetic terms, be able to smile confidently again, with a smile that is built and adapted to his individuality, in a structure that is completely fixed to his body, in his upper jaw and zygomatic bones.
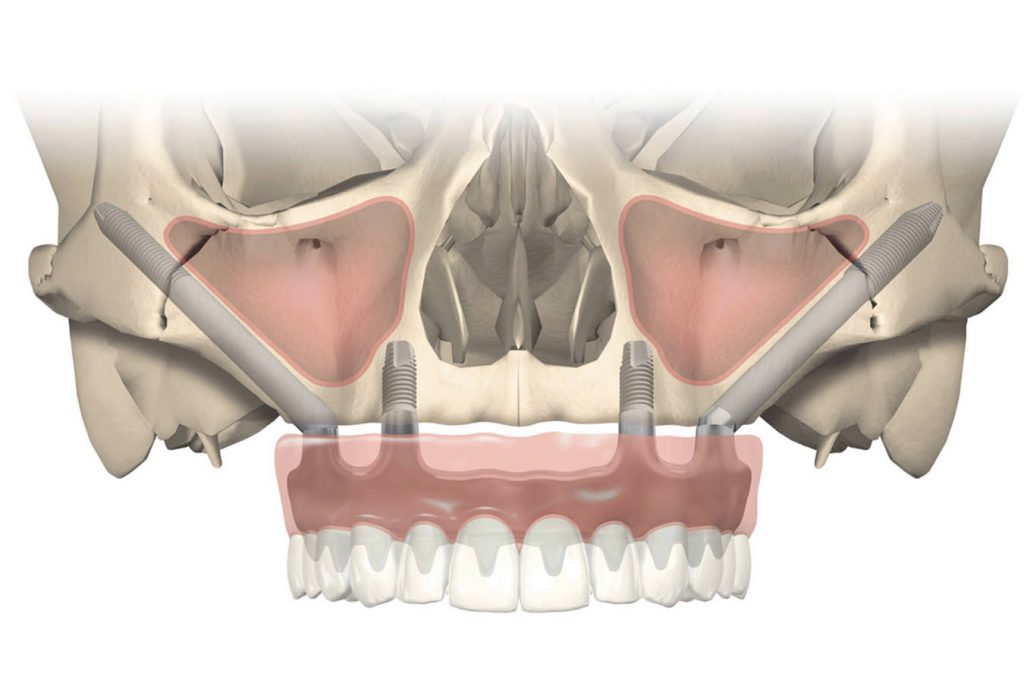
Zygomatic implants can be used in conjunction with conventional dental implants when there is still bone remaining in the upper jaw, i.e. in cases of moderate or advanced bone resorption that can be used by us as fixation during surgery, or in very extreme cases, i.e. in those cases where bone resorption is severe or extreme, where the fixation of the prosthetic structure will occur only in Zygomatic implants, where we use 2 Zygomatic implants on each side in the most extreme cases.


Who is a candidate for this type of treatment?
All patients in whom:
– Because the degree of bone resorption is so severe or extreme, performing maxillary bone grafts is no longer a viable treatment option, because one of the basic principles for performing a bone graft to increase the volume of bone, is to have enough remaining bone for the fixation of the bone graft.
– The medical and pathophysiological conditions allow this, which are measured with the set of medical, clinical, laboratory and radiology tests that we use for cases operated on under general anaesthesia. Our team operates on all patients for the placement of zygomatic implants in a hospital environment and under general anaesthesia. This therefore implies an anaesthetic consultation with our anaesthetic team.
– All Patients who have or have had failed rehabilitations in the mouth, and whose planning, technique or surgical approach has not been the most appropriate, the bone remaining after removal of the failed conventional dental implants is not of sufficient volume and quality in the upper jaw to be able to repeat the surgery and return to using only conventional dental implants.
By conventional dental implants, I mean those that have a normal size and shape, within the measurements and standards accepted internationally and scientifically by all the brands authorised to market dental implants, and which are applied to the Jawbone.
Zygomatic implants are not conventional because they are larger, mainly in terms of length, and although they pass through, are supported or even fixed in the upper jaw, their main anchorage is in the zygomatic bone.
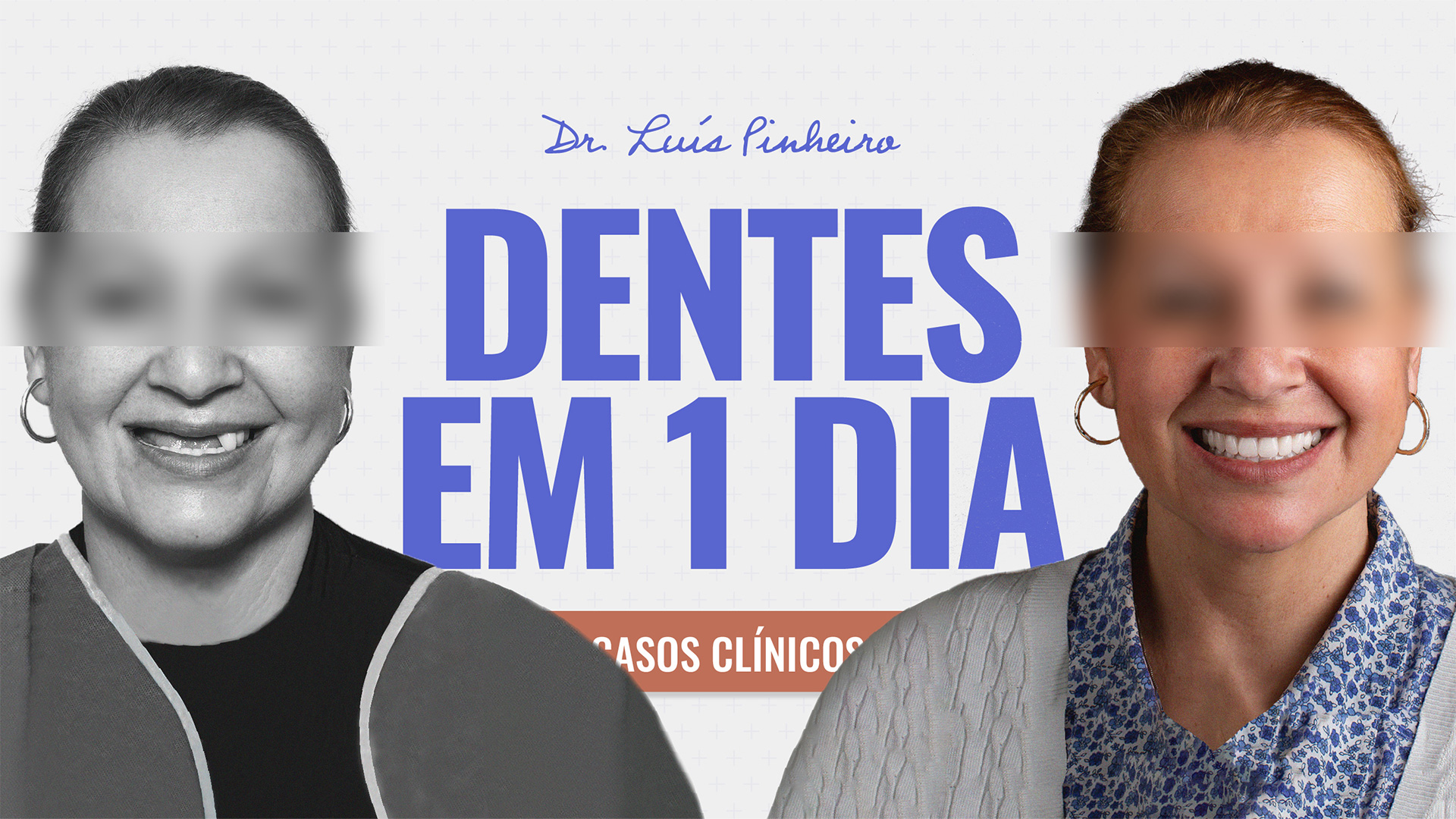
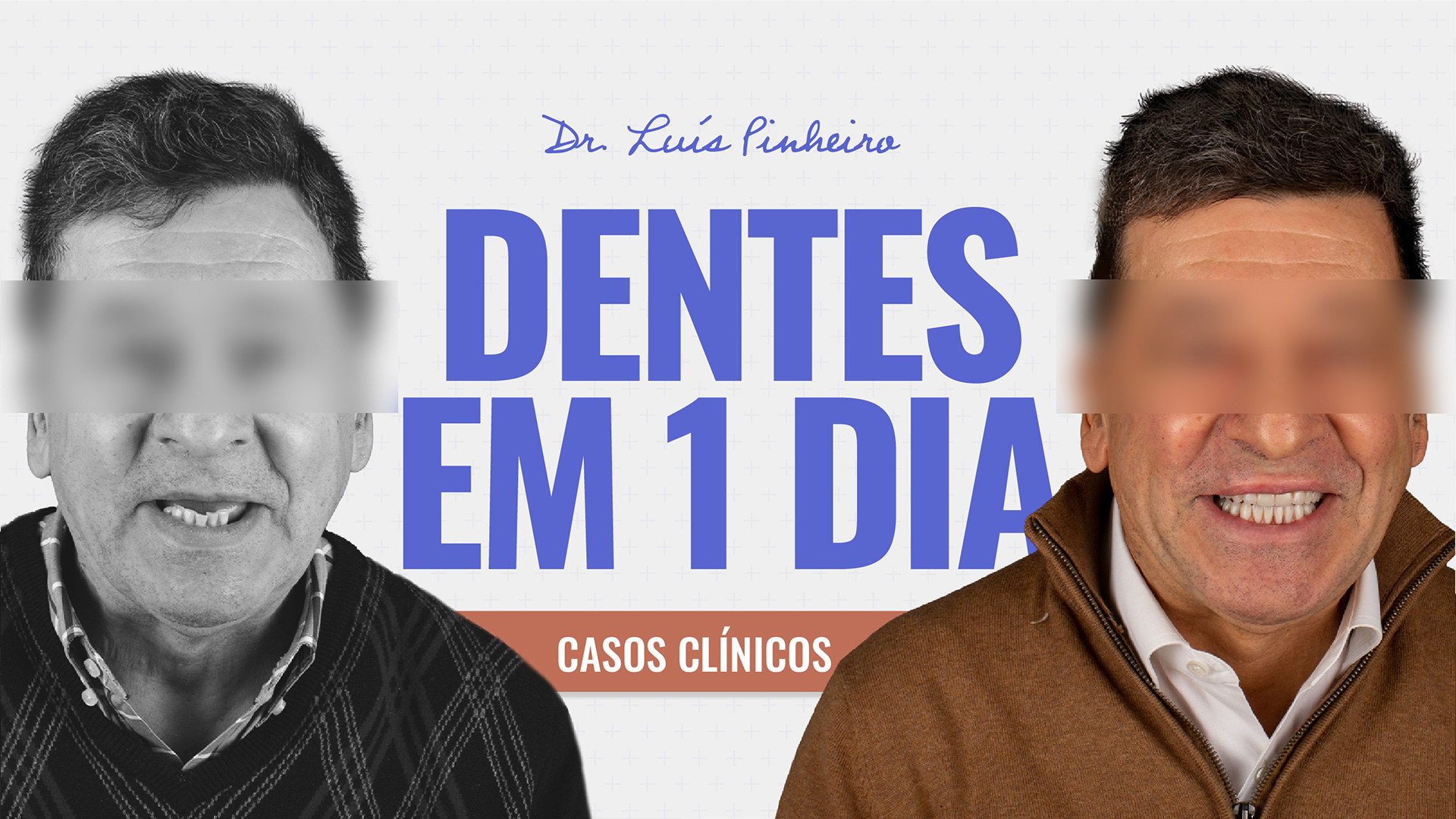
Clinical Case 1:
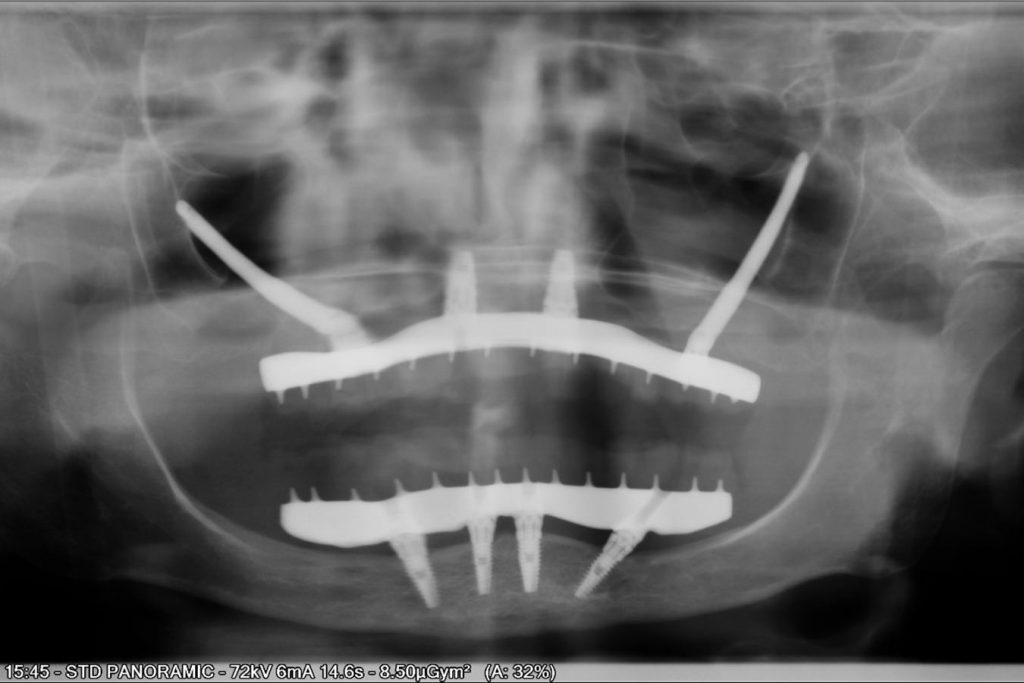
X-ray: Digital Orthopantomography
Patient M.F.F., female, 68 years old
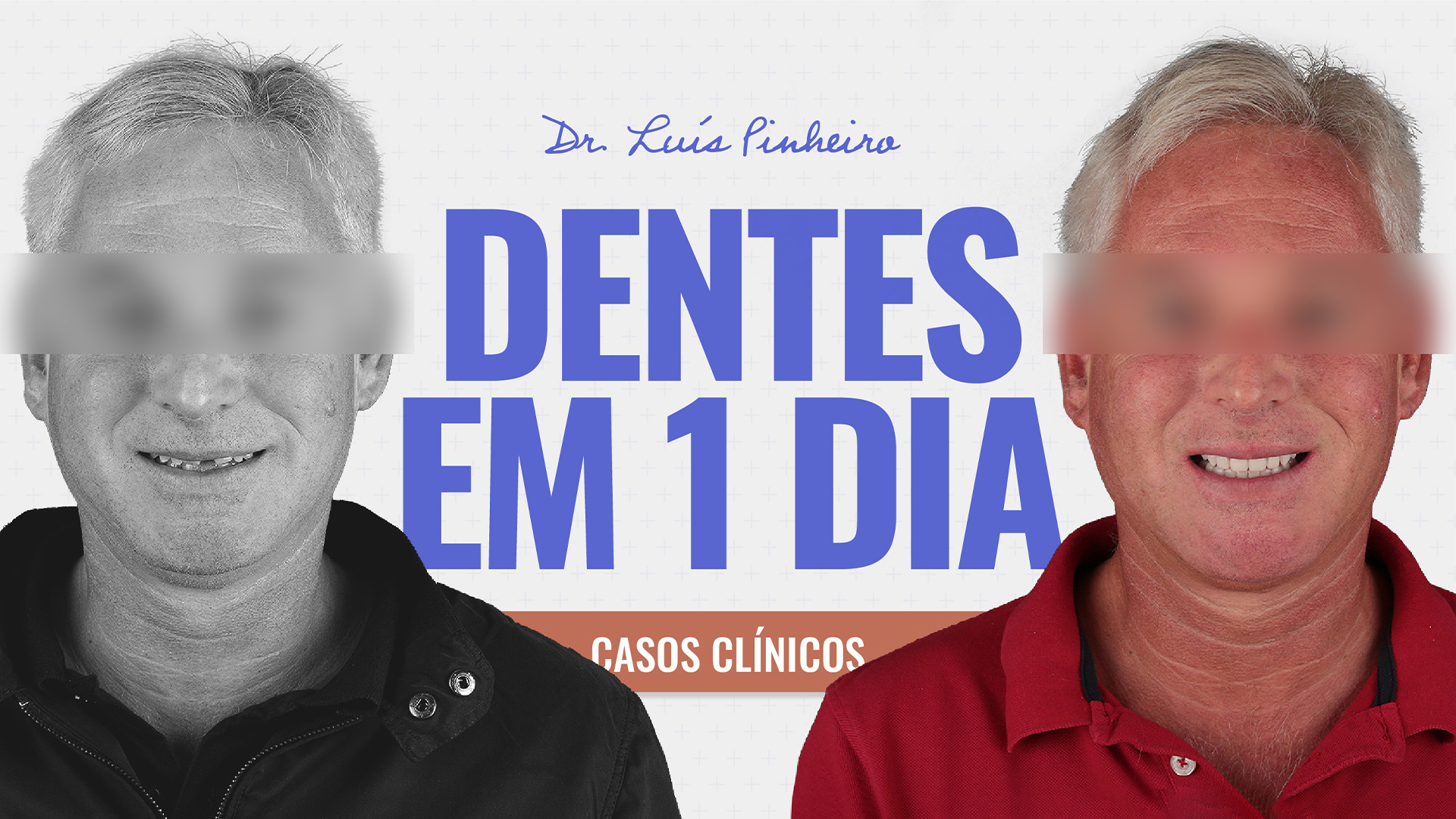
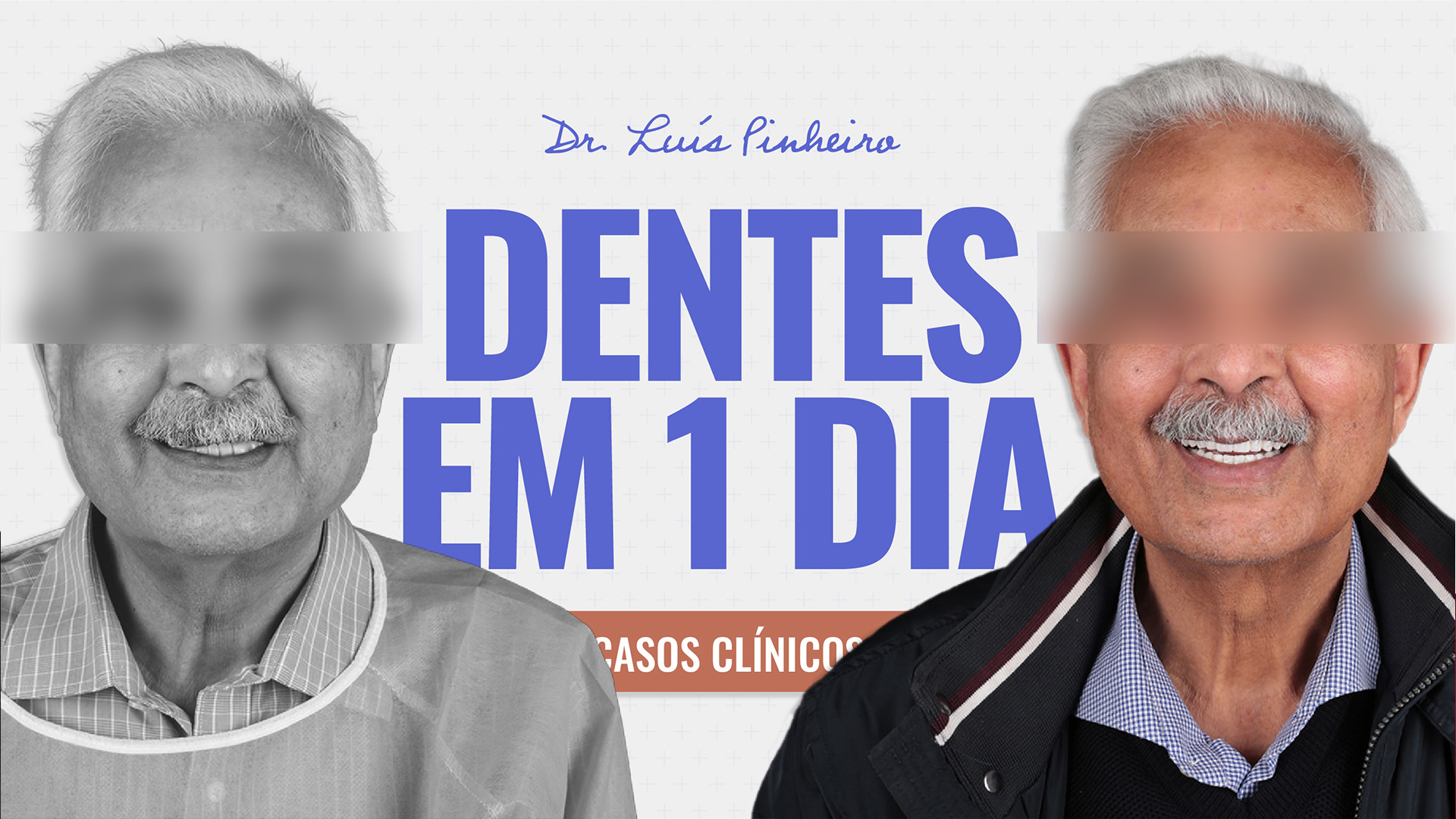
Clinical Case 2:
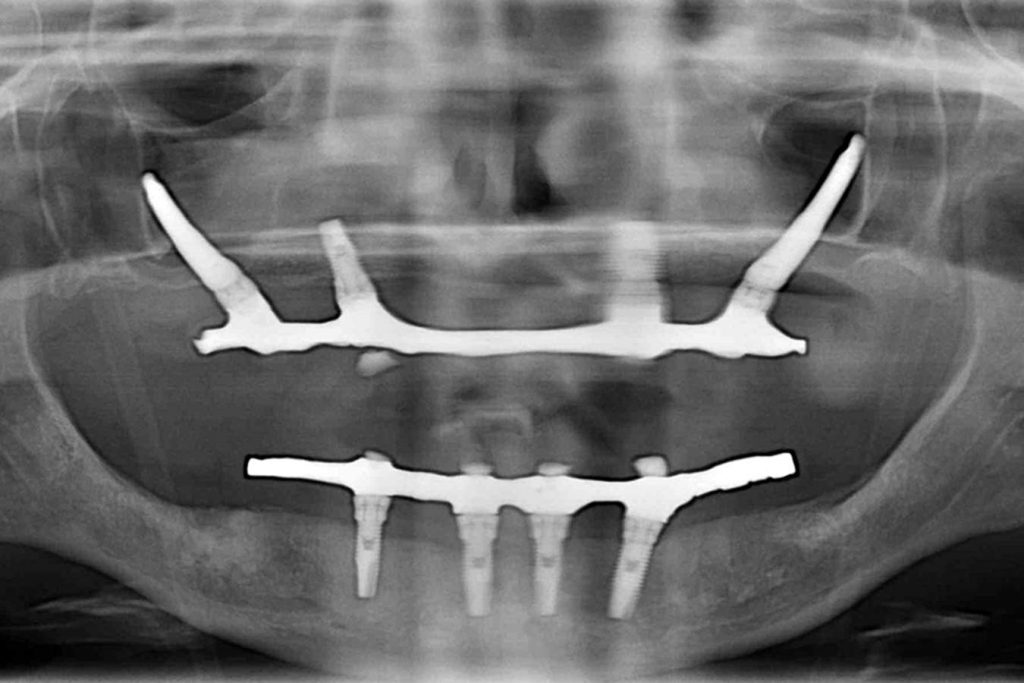
X-ray: Digital Orthopantomography
Patient C. R., female, 46 years old
It is a surgical technique that is performed on the mid-face, with an operating field that is larger than that of conventional maxillary surgery. It requires in-depth, qualified knowledge and specific techniques in its approach and should only be performed by highly trained and qualified doctors/surgeons whose curricula include specific training for this type of surgery.
Like any other, the technique has its risks and complications, which will be explained to you in detail by our medical and nursing team.
However, it is a well-studied, safe and predictable technique, performed by those who know how and with responsible patients who are able to fully understand and correctly carry out all the precautions.
When the bone allows us in terms of quality, quantity and safety in the implant insertion forces obtained (torque), the Surgery Team informs the Rehabilitation Team that it will be possible to rehabilitate the patient in immediate function, that is, to have the teeth screwed in the same day and from then on, it’s a “Teeth in 1 Day” situation like our other patients who are rehabilitated with our Conventional Dental Implants.
However, zygomatic implant surgeries are cases of severe and extreme bone resorption and there are many times when we don’t perform the immediate function of the implants, either zygomatic or conventional.
For a period of 6 to 8 months, the patient wears a Conventional Removable Complete Denture with a soft filling that is replaced every 3 weeks by our Rehabilitation Team. After this period of osseointegration, we can attach the new structures to the implants.
There was a lot more to say, a lot more to show, but I hope I’ve helped to enlighten our followers and readers about a subject that is very dear to me and that takes up a lot of my time in life, in its study, teaching, research and, of course, in surgery.
See you soon and don’t forget to be happy. After all, smiling doesn’t hurt…
If this is the case, if smiling causes you pain, nausea or imbalance, consult your dentist.
Until next time!